Abstract
Introduction
Incidence of Non-Hodgkin lymphoma (NHL) has been increasing steadily. Diffuse large B Cell Lymphoma (DLBCL) constitutes 30% of all NHLs. It can present as nodal or extra nodal disease. Based on other primary sites of origin, extra nodal DLBCL (EN-DLBCL) may have a distinct clinical outcome. Apart from site of origin, factors including demographics, staging and presence of other primary malignancy may also affect the outcome in these patients. Purpose of this study is to identify prognostically distinct groups, to lay the foundation for future studies aiming at tailored treatment based on the site of involvement.
Methods
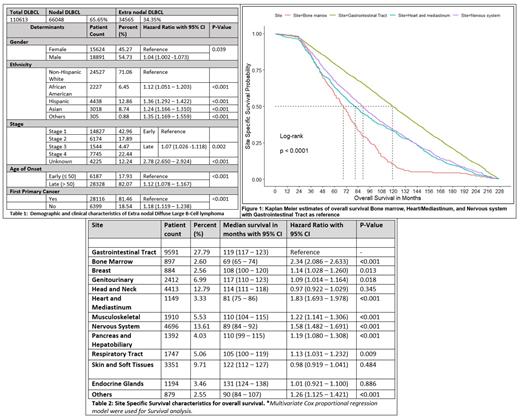
We identified patients in the Surveillance, Epidemiology and End Results (SEER) database who were diagnosed with DLBCL and EN-DLBCL from 2000 through 2016 based on the WHO ICD-O-3 classification. A total of 34565 EN-DLBCL patients were identified. Patients with unknown survival duration were excluded and accordingly 34515 patients were included for survival analysis. Survival analysis variables included gender, ethnicity, age of onset (Early ≤ 50, late >50 years), site of origin, staging of the tumor as early-stage (stage 1 and stage 2) or late-stage tumors (stage 3 and stage 4), and history of prior malignancy (first primary tumor or second/later primary tumor). There were 267 sites based on primary site code in the SEER database, which were grouped based on organ systems. Survival analysis was done using a cox-proportional hazard regression model. Site specific survival curves were estimated by the Kaplan-Meier method and were compared using the log-rank test for bone marrow, heart/mediastinum and nervous system, as these sites had worse outcomes with gastrointestinal tract as reference (Figure - 1). Site specific median overall survival was reported with 95% confidence interval.
Results
The percentage of EN-DLBCL of all DLBCL is 34.35%. Demographically, EN-DLBCL was most seen in Male (54.73%) and Non-Hispanic white (71.06%). In terms of clinical characteristics, patients with EN-DLBCL mostly had late age of onset, i.e. >/= 50 years (82.07%), Stage I disease (42.96%) and presentation as first primary cancer (81.46%). Higher risk of mortality was seen in Hispanic population (HR 1.36, 1.292-1.422) with non-Hispanic white as reference, late age of onset (HR 1.12, 1.078-1.167), late stage (III and IV) of presentation (HR 1.07, 1.026-1.118) and with history of any other malignancy (HR 1.18, 1.119-1.238) (Table - 1). Among EN-DLBCL, gastrointestinal tract (27.79%), nervous system (13.61%), head and neck (12.79%) and skin and soft tissue (9.71%) were the most common sites of origin. In the survival analysis, the risk of all-cause mortality was found to be higher in individuals with involvement of bone marrow (HR 2.34, 2.086-2.633), heart and mediastinum (HR 1.83, 1.693-1.978) and nervous system (HR 1.58, 1.482-1.691), with GI/Alimentary tract as reference (Table - 2).
Conclusion
Primary site of disease is an important prognostic factor for patients with EN-DLBCL after adjusting for confounders like age, sex, race and stage. Possible explanations to our findings include degree of vital organs affected, treatment modalities involved, risk of central nervous system (CNS) recurrence, immune status, and molecular biology. Unlike the typical DLBCL, Primary mediastinal/thymic large B cell lymphoma and primary CNS lymphoma has already been recognized as a separate entity in WHO classification, because of its specific behavior. Based on our population-based study, we conclude that there is a need for separate guidelines and tailored treatment for other primary extra nodal sites as well. Our study showed a worse outcome in Hispanic population when compared to other races. There is a need for further prospective studies to evaluate racial association with existing prognostic factors.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal